Cutaneous horn is one of those dermatological curiosities that often surprises people, especially those who have never heard of it. If you’re reading this, you’ve probably been diagnosed with this condition, know someone who has it, or simply found the topic interesting. Whatever the case may be, welcome. Here, I will explain what a cutaneous horn is, why it appears, and how it can be properly treated.
My name is Sebastian Podlipnik, I am a dermatologist at the Hospital Clínic of Barcelona, and I have spent years researching and treating various skin diseases, including those related to sun exposure and skin cancer. I have seen numerous cases of cutaneous horns, and my priority is always to ensure that patients understand what this condition is, why it occurs, and how to treat it effectively.
In this article, I will share my experience with you in a clear way so that you can better understand what it is and what steps to take if you ever encounter this lesion.
What will I talk about in this article?
What is a Cutaneous Horn?
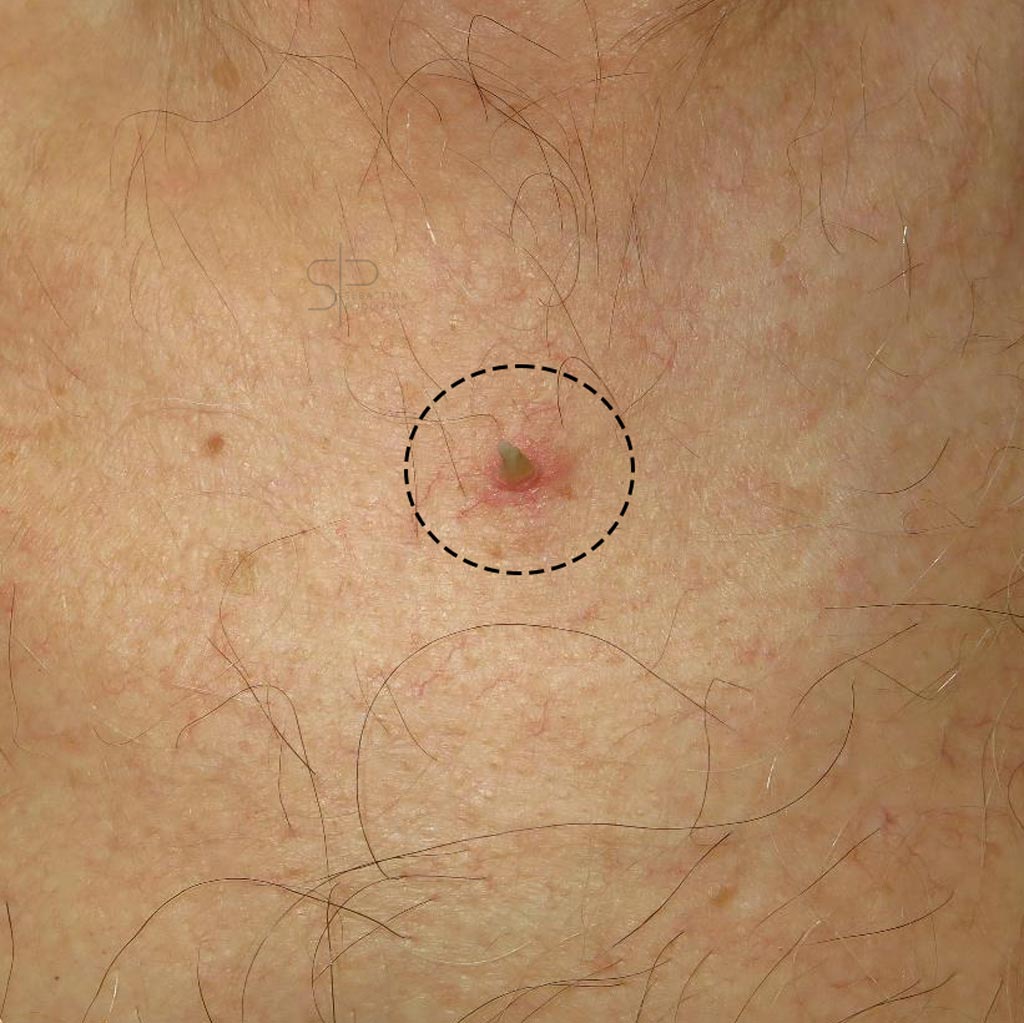
A cutaneous horn is a skin lesion that appears as a rigid protrusion or growth primarily made of keratin, the same protein that makes up our nails and hair. Visually, it can resemble a horn emerging from the skin, which is where its name comes from. Although its appearance may alarm some, the cutaneous horn is not a disease in itself, but rather a manifestation of an underlying skin problem.
These lesions vary in size, with some being small while others can reach several centimeters in length. A cutaneous horn can appear anywhere on the body, although it is more common in sun-exposed areas such as the face, scalp, ears, and hands. It affects both men and women, although it is more common in people over 60 years of age. (Copcu et al., 2004).

Why Does a Cutaneous Horn Form?
A cutaneous horn forms due to an accumulation of keratin in the skin, but this buildup is not random. It is related to an underlying skin lesion. This is crucial from a dermatological perspective, because although the horn itself may not be dangerous, it signals that benign, precancerous, or even malignant conditions could exist at the base of the cutaneous horn. (Bondeson, 2015).
Is a Cutaneous Horn Dangerous?
One of the most common questions I hear in consultations is whether a cutaneous horn is dangerous. The short answer is: it depends. Not all cutaneous horns are dangerous, but some can be secondary to a malignant lesion. What really matters is the base of the lesion, as I mentioned earlier. Many cutaneous horns develop over benign lesions, such as seborrheic keratosis, which are not dangerous. However, in other cases, the cutaneous horn may form over an actinic keratosis (a precancerous lesion), or, in more serious cases, over a squamous cell carcinoma, a type of skin cancer. (Reddy et al., 2013).
Cutaneous Horn and Skin Cancer
Cutaneous horns are most commonly associated with malignant lesions in people over the age of 50, especially those with prolonged sun exposure. In fact, recent studies suggest that around 20% of cutaneous horns are related to skin cancers, particularly squamous cell carcinoma. Therefore, although it is not always dangerous, it is essential that any cutaneous horn be evaluated by a dermatologist to rule out serious issues. (Yu et al., 2019).

How is a Cutaneous Horn Diagnosed?
The diagnosis of a cutaneous horn is usually straightforward due to its characteristic appearance. However, it is crucial to perform a biopsy in most cases to evaluate the underlying lesion. Through the biopsy, we can determine whether the base of the lesion is benign, precancerous, or malignant, which allows us to decide on the most appropriate treatment. (Meyerson et al., 2017).
When is a Biopsy Necessary?
I recommend a biopsy in most cases of cutaneous horn, especially if the patient has a history of prolonged sun exposure or skin cancer. The biopsy not only provides an accurate diagnosis but also gives us peace of mind by determining if there is an underlying risk that needs to be addressed. (Morgan et al., 2020). In some cases, a dermatoscopic examination of the lesion can help us make an accurate diagnosis and avoid a biopsy.

Treatment in Cases of Malignancy
When the biopsy reveals a malignant lesion, the treatment can be more complex. In some cases, a more extensive surgery (widening the margins) is necessary to ensure that all affected tissue is removed. This is particularly important in cases of squamous cell carcinoma. (Mounsey et al., 2018).
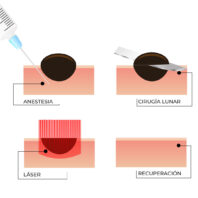
Treatment Options:
- Surgical Excision: The horn is removed along with the underlying lesion, and this is the method of choice in most cases.
- Cryotherapy: The lesion is frozen with liquid nitrogen to remove it. This is especially indicated if the cutaneous horn is related to benign lesions or actinic keratosis.
- Curettage and Electrodessication: It involves scraping the lesion and destroying the base with electric current. Like cryotherapy, it is reserved for cases of benign lesions or actinic keratosis.
- Photodynamic Therapy: It uses light and a photosensitizer to destroy precancerous cells and is used for premalignant lesions or squamous cell carcinoma in situ (located in the most superficial layer of the skin – the epidermis). (Simmons et al., 2017).
Prevention of Cutaneous Horn
Preventing the appearance of these lesions is closely related to sun protection. Most of the lesions that can produce a cutaneous horn are linked to accumulated sun damage, so protecting the skin is key to reducing the risk of developing cutaneous horns. (D'Orazio et al., 2016).
Prevention Tips:
- Apply sunscreen daily, even on cloudy days.
- Avoid sun exposure during peak hours.
- Wear protective clothing and wide-brimmed hats.
- Have regular dermatological check-ups, especially if you have a history of prolonged sun exposure.
Frequently Asked Questions About Cutaneous Horn
Is a Cutaneous Horn Always Malignant?
No, many cutaneous horns are benign, but they should always be evaluated by a dermatologist to rule out more serious issues.
How can I tell if I have a cutaneous horn?
A cutaneous horn appears as a hard protrusion on the skin, which can vary in size. If you have a lesion that looks like a horn, it is important to have it evaluated by a dermatologist.
Can a Cutaneous Horn Recur After Being Removed?
In some cases, if the underlying lesion is not completely removed, the cutaneous horn can reappear. That’s why it’s crucial to treat both the horn and the underlying tissue.
My Experience with Patients with Cutaneous Horn
Throughout my career as a dermatologist, I have treated many cases of skin cancer and cutaneous horns. What I have learned is that early detection and treatment are key to preventing major complications. I advise my patients to pay attention to any changes in their skin, especially in sun-exposed areas, and to consult a dermatologist if they have any concerns.
Conclusion
A cutaneous horn may seem like a simple curiosity, but its evaluation and treatment are essential to avoid complications. Whether benign or malignant, it should be assessed by a dermatologist to ensure proper treatment. Remember that prevention, especially through sun protection, is your best tool to avoid this type of lesion.
If you have more questions about cutaneous horns or other dermatological conditions, feel free to leave your comment below, and if you have one, don’t hesitate to request a consultation. I’m here to help you take care of your skin.